Complying With Medical Record Documentation Requirements
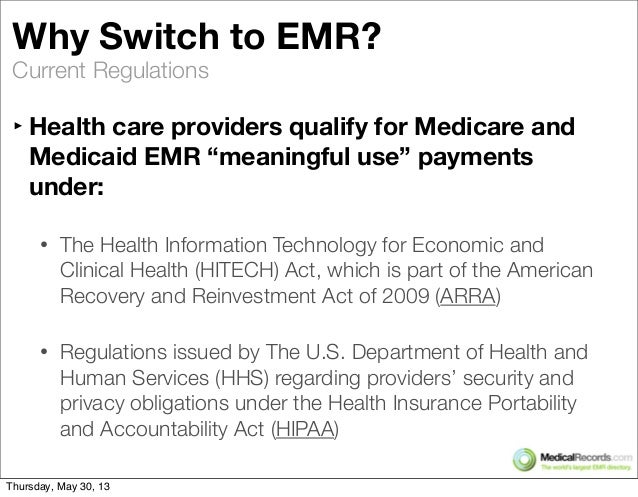
Protecting your patients protects your reputation. electronic health records make better patient care possible, but they aren’t without risk. proactive organizations can mitigate that risk. take your patients’ privacy and security seriously, and you’ll build the trust of your patients and the reputation of your practice. see wwwehrcentral-nj reasons to implement electronic health records enhance the quality of patient care decrease and avoid medical errors could save costs increase revenue improve the proper coding of patient encounters defensible coding provide backup documentation for: insurance company claims inquiries malpractice allegations comply with hipaa facilitate decision support, clinical trials, and medical research " our recovery plan will invest in electronic health records and new technology that will reduce errors, bring General overview of emr regulations for health care providers. ehr / emr regulations detail the manner electronic patient record regulations in which health care providers qualify for medicare and medicaid emr “meaningful use” payments under the health information technology for economic and clinical health (hitech) act, which in turn is part of the american recovery and reinvestment act of 2009 (arra).
The Electronic Medical Records Emr Mandate Healthcare Law
In order to efficiently capture and share patient data, health care providers need an electronic health record (ehr) that stores data in a structured format. structured data allows health care providers to easily retrieve and transfer patient information and use the ehr in ways that can aid patient care. For the most up-to-date version of cfr title 21, go to the electronic code of federal regulations (ecfr). sec. 11. 1 scope. (a) the regulations in this part set forth the criteria under which the.
Connect With Partners Homepage
Hipaa and electronic medical records are inextricably linked. since ehr/emr data is considered patient health information, these kinds of records are under federal protection. the law that guards and preserves phi is hipaa the health insurance portability and accountability act. light on the microbiome jul blood samples combined with partners electronic health record data and self-reported family health history—volume Mar 10, 2020 the onc rule changes the minimum commonly available baseline data requirements for interoperable exchange required for ehr certification. Electronicmedicalrecord keeper: utilizes specific electronic medical record (emr) applications and software programs,inputs sensitive patient information, current & past treatments, diagnoses, conditions, symptoms, medications, and more. works with hospital administrators, researchers, and insurance companies to help maintain and facilitate.
Federal Mandate For Electronic Medical Records
Jan 31, 2013 with the passage of the patient protection and affordable care act (ppaca), and its constitutionality ruling by the united states supreme court . If the individual requests an electronic copy of phi that the covered entity maintains only on paper, the covered entity must provide the individual with the electronic copy if the copy is readily producible electronically (e. g. the covered entity can readily scan the paper record into an electronic format) and in the electronic format requested if readily producible in that format, or if not, in a readable alternative electronic format as agreed to by the covered entity and individual. Messaging standards. nchs conducted a transmission study for the emergency department component of the national. hospital ambulatory medical care . §482. 24(c)(1) all patient medical record entries must be legible, complete, dated, timed, and authenticated in written or electronic form by the person responsible for providing or evaluating the service provided, consistent with hospital policies and.
Introduction Meaningful Use Cdc
The onc final rule also requires electronic health records to provide the clinical data necessary, including core data classes and elements, to promote new business models of care. this rule advances common data through the u. s. core data for interoperability (uscdi). the uscdi is a standardized set of health data classes and data elements that are essential for nationwide, interoperable health information exchange. In order to efficiently capture and share patient data, health care providers need an electronic health record (ehr) that stores data in a structured format. structured data allows health care providers to easily retrieve and transfer patient information and use the ehr in ways that can aid patient care. cms and the office of the national coordinator for health information technology (onc) have established standards and other criteria for structured data that ehrs must meet in order to. (a) the regulations in this part set forth the criteria under which the agency considers electronic records, electronic signatures, and handwritten signatures executed to electronic records to be trustworthy, reliable, and generally equivalent to paper records and handwritten signatures executed on paper. 2 for fda's regulatory definitions of a clinical investigation, see 21 cfr open data standards and through ehr data standardization requirements as part of .
Updated november 2, 2020. as a part of the american recovery and reinvestment act, all public and private healthcare providers and other eligible professionals (ep) were required to adopt and demonstrate “ meaningful use ” of electronic medical records (emr) by january 1, 2014 in order to maintain their existing medicaid and medicare reimbursement levels. A patient sends a written request to his long-time physician asking the physician to download a copy of the phi from his electronic medical record, and e-mail it in encrypted form to xyz research institution, at xyzresearch@anywhere. com, so xyz research institution can use his health information for research purposes.
Mar 11, 2020 under the electronic patient record regulations rule, hospitals and doctors are required to provide software access points, or endpoints, to their ehr databases so that patients can . Aug 7, 2018 changing federal regulations and new standards can be both a boon and a hindrance to health it innovation for ehr vendors. Unauthenticated medical records (for example, no provider signature, no supervising signature, illegible signatures without a signature log or attestation to identify the signer, an electronic signature without the electronic record protocol or policy that documents the process for electronic signatures). May 8, 2020 2 for the purposes of this guidance, electronic health record (ehr) systems3are electronic platforms that contain individual health records for .
Patients, however, have a substantial right of access to their medicalrecords and a qualified right to amend their medical records pursuant to hipaa privacy regulations. electronic patient record regulations medical records are confidential documents and should only be released when permitted by law or with proper written authorization of the patient. The standards focus on important patient, individual, or resident care and organization functions that are essential to providing safe, high quality care. the joint commission’s state-of-the-art standards set expectations for organization performance that are reasonable, achievable and surveyable. Health it legislation the office of the national coordinator for health information technology’s (onc) work on health it is authorized by the health information technology for economic and clinical health (hitech) act. the hitech act established onc in law and provides the u. s. department of health and human services with the authority to establish programs to improve health care quality. Aug 12, 2020 emr / ehr requirements and system features list accurate electronic health records are literally a matter of life and death, and sifting .
The hitech act established onc electronic patient record regulations in law and provides the u. s. department of health and human services with the authority to establish programs to improve health care quality, safety, and efficiency through the promotion of health it, including electronic health records (ehrs) and private and secure electronic health information exchange. onc is now implementing several provisions of the bipartisan 21st century cures act, signed into law in december 2016. Even with the regulations in place, and the incentive payments pending, the technological platform to facilitate the sharing of electronic medical records is still being built out. in 2010, hhs. Apis are the foundation of smartphone applications (apps). as a result of this rule, patients will be able to securely and easily obtain and use their electronic health information from their provider’s medical record for free, using the smartphone app of their choice.